New standard neoadjuvant therapy of pancreatic cancer (CASSANDRA)
Reni M et al, Lancet. 2026;406(10522):2945-2956
In a randomized phase 3 trial on preoperative therapy of pancreatic carcinoma, treatment according to the PAXG protocol (capecitabine, cisplatin, nab-paclitaxel, and gemcitabine) resulted in a significantly longer event-free survival as compared to treatment with mFOLFIRINOX (fluorouracil, leucovorin, irinotecan, and oxaliplatin) and could therefore be considered a new standard option.
Background: Perioperative chemotherapy is a standard option for treatment of patients with resectable and borderline resectable pancreatic ductal adenocarcinoma (PDAC). This study aimed to assess the superiority of PAXG (cisplatin, nab-paclitaxel, capecitabine, and gemcitabine) over mFOLFIRINOX (modified fluorouracil, leucovorin, irinotecan, and oxaliplatin) in this population.
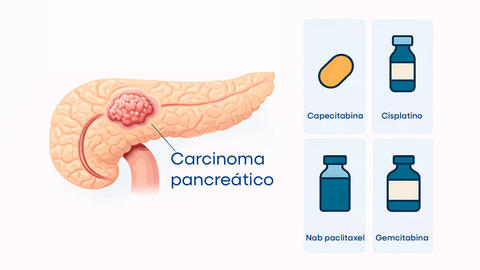
Methods: CASSANDRA is a randomised, open-label, 2 × 2 factorial phase 3 trial, involving 17 Italian academic hospitals. Eligible patients were aged 18–75 years with pathologically confirmed resectable or borderline resectable PDAC. Randomisation was performed by a central web-based system using R-code lists with a computerised algorithm. The design adopted a 1:1 randomisation, with a block stratification by centre and carbohydrate antigen 19-9. Participants were first randomly assigned PAXG (total daily capecitabine dose of 1250 mg/m2 in a 625 mg/m2 twice a day dosage and intravenous cisplatin 30 mg/m2, nab-paclitaxel 150 mg/m2, and gemcitabine 800 mg/m2 every 14 days) or mFOLFIRINOX (intravenous fluorouracil 2400 mg/m2, leucovorin 400 mg/m2, irinotecan 150 mg/m2, and oxaliplatin 85 mg/m2 every 14 days) for 4 months, followed by a second randomisation to 2 months of additional chemotherapy either before or after surgery. The primary endpoint was event-free survival (EFS) in the intention-to-treat population and the safety population included all patients who received at least one cycle of the assigned therapy. The results of the first randomisation are reported here.
Findings: Between November 3, 2020, and April 24, 2024, 132 eligible patients were assigned to PAXG and 128 to mFOLFIRINOX. In the PAXG group, the median age was 65 years (IQR, 60–70), 68 (52%) of 132 patients were female, and 64 (48%) were male. In the mFOLFIRNOX group, the median age was 63 years (IQR, 57–69), 62 (48%) of 128 patients were female, and 66 (52%) were male. All 260 patients received at least one assigned chemotherapy administration. PAXG prolonged the median EFS compared with mFOLFIRINOX (16.0 months [95% CI: 12.4–19.8] vs. 10.2 months [8.6–13.5]; hazard ratio = 0.63 [0.47–0.84]; p = 0.0018). At least one grade 3 or worse adverse event was observed in 87 (66%) of 132 patients in the PAXG group and in 78 (61%) of 128 patients in the mFOLFIRINOX group, including one fatal event.
Interpretation: PAXG significantly improved EFS compared with mFOLFIRINOX in resectable or borderline resectable PDAC. Preopertive PAXG could be considered a standard option for resectable or borderline resectable PDAC. Accordingly, preoperative PAXG should be considered as the standard comparator group for future trials in this setting.