Guselkumab for the treatment of ulcerative colitis
Rubin DT et al, Lancet. 2025;405(10472):33-49
In this phase 3 study in patients with moderate to severe ulcerative colitis (QUASAR), 23% achieved clinical remission after 12 weeks of treatment with the IL-23 antibody guselkumab compared to 8% with placebo. During maintenance therapy, 50% of patients treated with guselkumab achieved clinical remission after 44 weeks.
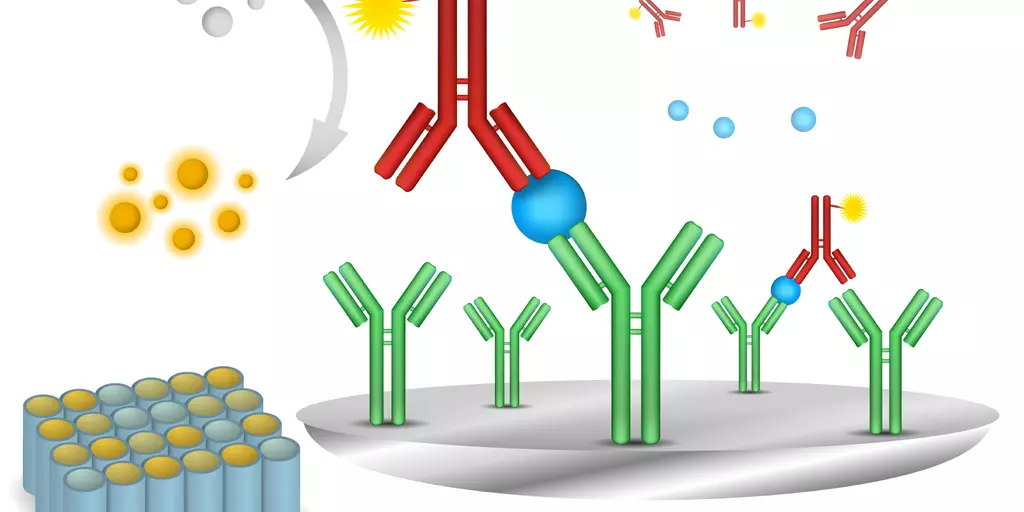
Background: Interleukin-23 inhibition is effective in treating ulcerative colitis. Guselkumab is a dual-acting, human IgG1, interleukin-23p19 subunit inhibitor that potently neutralises interleukin-23 and can bind to CD64. The aim of this study was to evaluate the efficacy and safety of guselkumab as induction and maintenance therapy in patients with ulcerative colitis.
Methods: The primary populations of these 2 phase 3, randomised, double-blind, placebo-controlled studies (QUASAR phase 3 induction and maintenance) included randomised and treated adults with moderately to severely active ulcerative colitis (induction baseline modified Mayo score from 5 to 9) with inadequate response or intolerance to conventional or advanced ulcerative colitis therapy. Patients were randomly assigned (3:2) to receive guselkumab 200 mg given intravenously or placebo at weeks 0, 4, and 8 (phase 3 induction study). All patients were randomly assigned using web-based interactive response technology. Patients in clinical response 12 weeks after guselkumab induction given intravenously (from QUASAR phase 2b and phase 3 induction studies) were randomly assigned (1:1:1) at maintenance week 0 to guselkumab 200 mg given subcutaneously every 4 weeks or 100 mg every 8 weeks or placebo for 44 weeks (maintenance). Primary endpoints were clinical remission at induction week 12 and maintenance week 44.
Findings: The induction study primary population included 701 patients (guselkumab 200 mg given intravenously 60% [421 patients]; placebo 40% [280 patients]). The maintenance study primary population included 568 guselkumab induction responders randomly assigned to receive guselkumab 200 mg given subcutaneously every 4 weeks (190 patients [33%]) or 100 mg every 8 weeks (188 patients [33%]) or placebo (guselkumab withdrawal 190 patients [33%]). A significantly greater proportion of patients treated with guselkumab given intravenously had clinical remission at induction week 12 (23% [95/421 patients]) than did placebo-treated patients (8% [22/280 patients]; adjusted treatment difference 15%, 95% confidence interval [CI]: 10–20; p < 0.0001). Clinical remission at maintenance week 44 was achieved by a significantly greater proportion of patients treated with guselkumab 200 mg given subcutaneously every 4 weeks (50% [95/190 patients]; adjusted treatment difference 30%, 95% CI: 21–38; p < 0.0001) and 100 mg every 8 weeks (45% [85/188 patients]; adjusted treatment difference 25%, 95% CI: 16–34; p < 0.0001) than with placebo (19% [36/190 patients]). The overall safety profile was favourable and consistent with that of guselkumab in approved indications. In the induction study, adverse events were reported by 49% of patients in both groups (208/421 guselkumab-treated patients and 138/280 placebo-treated patients), serious adverse events were reported by 3% (12/421) of guselkumab-treated patients and 7% (20/280) of placebo-treated patients, and adverse events leading to treatment discontinuation were reported by 2% (7/421) of guselkumab-treated patients and 4% (11/280) of placebo-treated patients. In the maintenance study, adverse event rates were similar among groups, and the most frequently reported adverse events in all groups were ulcerative colitis, COVID-19, and arthralgia. No active tuberculosis, anaphylaxis, serum sickness, or clinically important hepatic disorders were reported in either study.
Interpretation: Guselkumab was effective and safe as induction and maintenance therapy in patients with moderately to severely active ulcerative colitis.