Endoscopic versus surgical gastroenterostomy for palliation of malignant outlet obstruction
van de Pavert YL et al, Lancet Gastroenterol Hepatol. 2025;10(12):1065-1074
In this randomized trial with patients suffering from malignant gastric outlet obstruction (ENDURO), palliative treatment with endoscopic gastroenterostomy was superior to surgical gastroenterostomy for time of resumption of solid oral intake and non-inferior for the rate of persistent or recurrent obstructive symptoms.
Background: In patients with malignant gastric outlet obstruction, endoscopic ultrasonography-guided gastroenterostomy might be superior to surgical gastroenterostomy, but randomised trials are scarce. The trial aimed to assess time to resumption of oral intake and the rate of persistent or recurrent obstructive symptoms requiring re-intervention following endoscopic ultrasonography-guided gastroenterostomy compared with surgical gastroenterostomy.
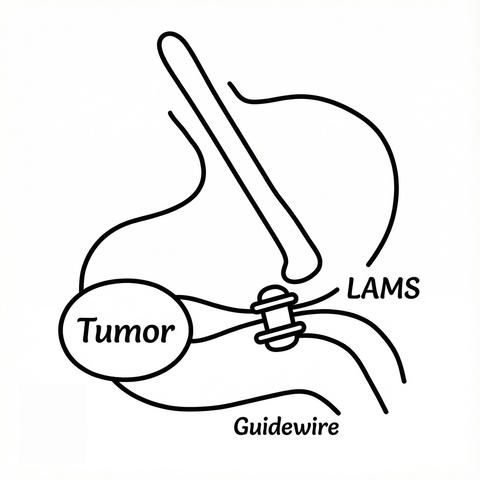
Methods: ENDURO was a multicentre, randomised controlled trial conducted at 12 Dutch academic and teaching hospitals. Hospitals with experience in at least 20 LAMS placements of any indication, at least ten endoscopic gastroenterostomies, and approved competence were eligible to perform endoscopic gastroenterostomy independently within the trial. Adults aged 18 years and older with symptomatic, malignant gastric outlet obstruction in a palliative setting were randomly assigned (1:1) to endoscopic or surgical gastroenterostomy. Randomisation was performed with an electronic data capture system using randomly generated permuted blocks of 2 and 4 and stratified by WHO performance status (0–1 and 2–3). The first coprimary outcome was time to resumption of solid oral intake (Gastric Outlet Obstruction Scoring System score ≥ 2). The second coprimary outcome was non-inferiority for persistent or recurrent obstructive symptoms requiring re-intervention. The predefined non-inferiority margin of the risk difference was 20%. All outcomes were analysed in all randomly assigned participants.
Findings: Between February 18, 2022, and February 26, 2024, 250 patients were screened, 98 of whom were randomly assigned to endoscopic gastroenterostomy (n = 48) or surgical gastroenterostomy (n = 50). 43 (44%) patients were female and 55 (56%) were male. Endoscopic gastroenterostomy had a shorter time to solid oral intake than surgical gastroenterostomy (median 1 day [IQR, 1–3] vs. 3 days [1–6], hazard ratio = 2.21 [95% CI: 1.43–3.42]; p = 0.0003). Endoscopic gastroenterostomy was non-inferior to surgical gastroenterostomy for persistent or recurrent obstructive symptoms requiring re-intervention (5 [10%] vs. 6 [12%], risk difference 1.6% [upper limit of 90% CI: 8.9]). Overall adverse events were reported in 28 (58%) patients in the endoscopic gastroenterostomy group and 32 (64%) in the surgical gastroenterostomy group (relative risk 0.91 [95% CI: 0.66–1.25]). One fatal event occurred in the endoscopic gastroenterostomy group and three fatal events occurred in the surgical gastroenterostomy group.
Interpretation: In patients with malignant gastric outlet obstruction, palliative treatment with endoscopic gastroenterostomy was superior to surgical gastroenterostomy for time to resumption of solid oral intake and was non-inferior for the rate of persistent or recurrent obstructive symptoms requiring re-intervention. Based on these results, endoscopic gastroenterostomy should be the preferred palliative treatment for patients with malignant gastric outlet obstruction.