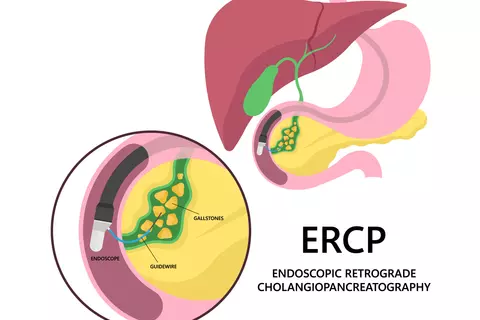
Adverse events associated with endoscopic retrograde cholangiopancreatography (ERCP)
Bishay K et al, Gastroenterology. 2025;168(3):568-586
A comprehensive meta-analysis of 380 trials with > 2 million patients revealed an overall incidence of post-ERCP pancreatitis of 4,6%, ERCP-related mortality of 0,2% and significant bleeding of 1,5%. Despite efforts to prevent post-ERCP pancreatitis, its incidence was static over the last 20 years.
Background and aims: Endoscopic retrograde cholangiopancreatography (ERCP)-related adverse events (AEs) are associated with morbidity, mortality, and health care expenditure. The aim of this study was to assess incidences and comparisons of ERCP AEs.
Methods: The authors included studies performed after 2000 reporting on ERCP AEs from database inception through March 12, 2024. Outcomes included pancreatitis, bleeding, cholangitis, cholecystitis, perforation, and death. DerSimonian and Laird random effects meta-analyses were performed to calculate incidences of AEs. Subgroup and pairwise meta-analyses were performed. Meta-regression was performed on median recruitment year to assess temporal trends in pancreatitis incidence.
Methods: The authors included studies performed after 2000 reporting on ERCP AEs from database inception through March 12, 2024. Outcomes included pancreatitis, bleeding, cholangitis, cholecystitis, perforation, and death. DerSimonian and Laird random effects meta-analyses were performed to calculate incidences of AEs. Subgroup and pairwise meta-analyses were performed. Meta-regression was performed on median recruitment year to assess temporal trends in pancreatitis incidence.
Results: A total of 380 studies were included. The incidence of death attributable to ERCP was 0.2% (95% confidence interval [CI]: 0.1–0.3%; I2, 44%; n = 47,258) in all-comers. The overall incidence of pancreatitis was 4.6% (95% CI: 4.0–5.1%; I2, 96%; n = 293,378) among all-comers and 6.5% (95% CI: 5.9–7.1%, I2, 89%; n = 88,809) among first-time patients. Pancreatitis incidence remained stable between 2000 and 2023 (average annual percent change 0.06, 95% CI: -0.27 to 0.39). The overall incidences of the following AEs for all-comers were: bleeding (1.5%; 95% CI: 1.2–1.7%; I2, 93%; n = 229,655), cholangitis (2.5%; 95% CI: 1.9–3.3%; I2, 96%; n = 121,619), cholecystitis (0.8%; 95% CI: 0.5–1.2%; I2, 39%; n = 7799), and perforation (0.5%; 95% CI: 0.4–0.6%; I2, 90%; n = 306,378).
Conclusions: Endoscopic retrograde cholangiopancreatography (ERCP)-associated adverse events remain common. Incidence of post-ERCP pancreatitis remained static despite improvements in techniques, prevention, and recognition. These results are important to patients, endoscopists, and policy makers to inform consent and to encourage implementation of available risk mitigation strategies.